Periodontal (Gum) Disease
Studies by the Centers for Disease Control and Prevention have found that more than 47% of US adults over the age of 30 have some form of periodontal disease. The earliest sign of periodontal disease is bleeding gums after brushing or flossing. If left untreated, periodontal disease can lead to tooth loss and have negative impacts on your overall health status.
Etiology
The primary cause of periodontal disease is a build-up of bacteria and food around the teeth and gums. Over time a sticky film traps food and more bacteria, leading to inflammation of the gum tissue, known as gingivitis. If the stick film or plaque are not removed, gingivitis can progress to periodontitis, a more severe form of the disease that can cause bone loss around the teeth and eventual tooth loss.
One of the hallmark symptoms of periodontal disease is bleeding gums, which occurs when the gums become inflamed and irritated by the bacteria in the plaque. Over time, this inflammation can lead to the breakdown of the connective tissue and bone that support the teeth, causing them to become loose and potentially fall out.
Treatment
The main goal in the treatment of periodontal disease is to remove the bacterial source of infection, and to rebuild the bone that may have been lost around your teeth. The initial steps may involve control of medical conditions, reviewing brushing and flossing habits, and an initial deep cleaning phase.
In more severe cases, additional deeper cleanings may be necessary to access and restore the original condition of the gums and bone around your teeth. Controlling active periodontal disease is a crucial step prior to any surgical periodontal treatment such as dental implants, crown lengthening, gum grafting, or bone grafting - maintaining periodontal health throughout your treatment will ensure a predictable and stable long-term outcome.
Your dentist will periodically measure the probing (pocket) depths around your teeth using a probe to check for signs of periodontal disease. Pocket depths tell us about the amount bone supporting our teeth.
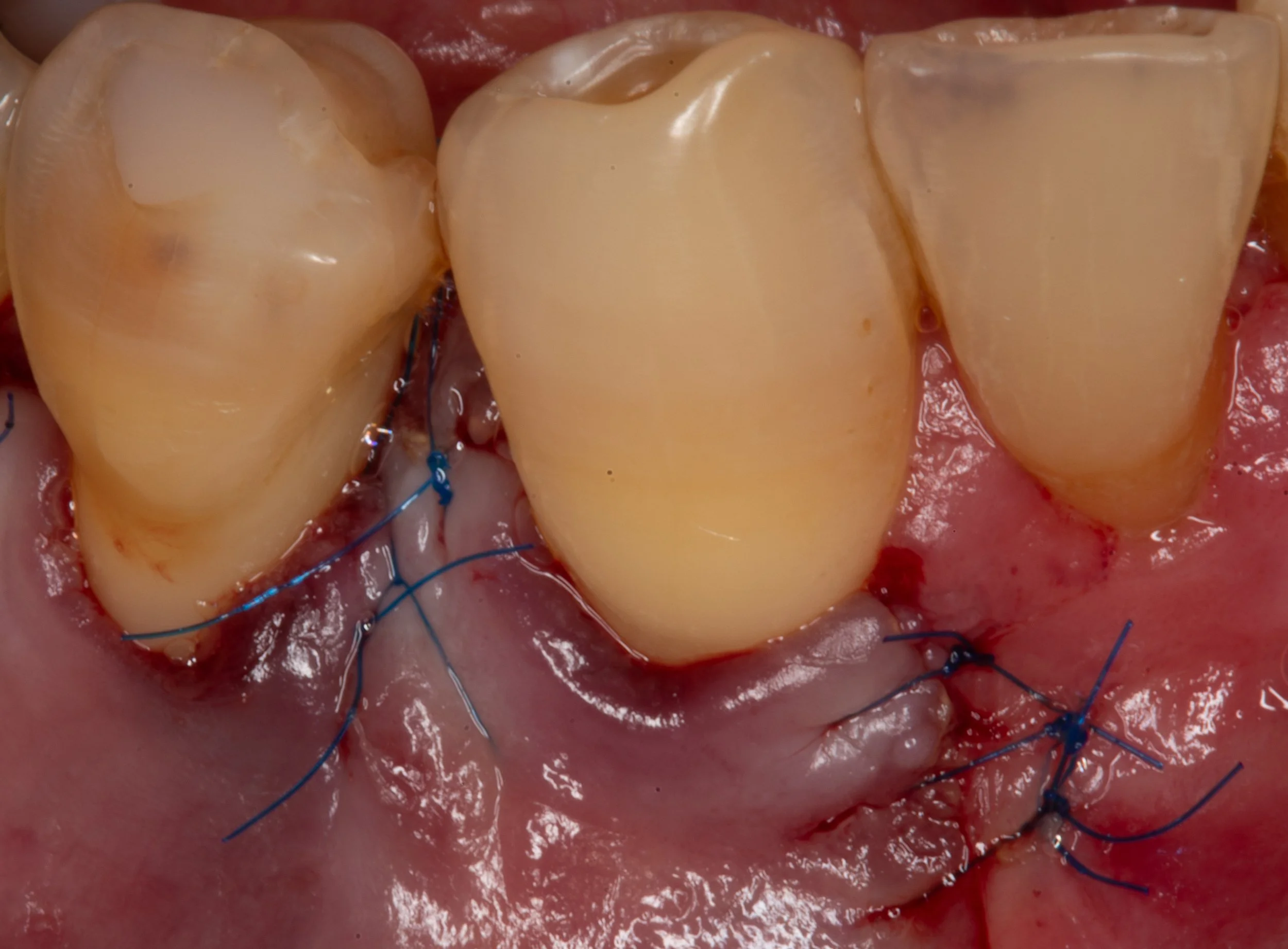
The pocket depth around a healthy tooth is between 1-3 millimeters. In the image above, the periodontal probe measured a 9 millimeter pocket depth around this tooth with heavy bleeding and gum inflammation (gingivitis).
When pocket depths measure greater than 4 millimeters, this suggests that periodontal disease and bone loss have occurred. The cause of bone loss around this tooth is bacteria that have collected under the gums and on the tooth. It is seen here on the tooth (brown spot), and has caused severe bone loss around the tooth.
Periodontal disease will cause more bone loss until the bacteria have been removed. In this scenario, a bone graft was obtained from a tissue bank and used to rebuild the lost bone and tooth support.
Sometimes periodontal disease and bone loss can be seen on the x-rays taken by your dentist (red dashed line). After bacteria have been removed from the tooth and a bone graft has been placed, the radiographic defect is no longer visible.
The treatment of periodontal disease is generally performed under local anesthesia in an outpatient setting. Initial healing can be expected in 2-weeks with minimal discomfort and interruption to your daily activities. Complete healing and return to regular, frequent cleanings is expected after 3-4 months.
Periodontal Disease
Periodontal disease is a chronic inflammatory condition that affects the tissues that surround and support each tooth. This includes the gums, ligaments, and bone. The etiology, or underlying cause of periodontal disease is multifactorial and involves a complex interplay between oral bacteria, the immune system, and other risk factors.
Characterized by swollen, bleeding gums and destruction of the bone around teeth, this process may progress unless the diseased, oral bacteria have been removed from beneath your gums. Once bone loss occurs, periodontal pockets form around your teeth for additional bacteria and food to accumulate.
Etiology:
The primary cause of periodontal disease is the accumulation of bacterial plaque on the teeth and gums. Plaque is a sticky film of bacteria that forms on the teeth and can cause inflammation of the gum tissue, known as gingivitis. If left untreated, gingivitis can progress to periodontitis, a more severe form of the disease that can cause bone loss around the teeth and eventual tooth loss.
One of the hallmark symptoms of periodontal disease is bleeding gums, which occurs when the gums become inflamed and irritated by the bacteria in the plaque. Over time, this inflammation can lead to the breakdown of the connective tissue and bone that support the teeth, causing them to become loose and potentially fall out.
The bacteria that cause periodontal disease are part of the normal oral microbiome, but certain species of bacteria can become more dominant in the presence of poor oral hygiene or other risk factors, such as smoking, diabetes, or genetic predisposition. These bacteria can produce toxins that further damage the gums and bone, exacerbating the inflammatory response.
In addition to bacteria, other factors that can contribute to the development of periodontal disease include hormonal changes, medications that reduce saliva flow, and certain systemic diseases. All of these factors can disrupt the balance of bacteria in the mouth and make it easier for harmful bacteria to thrive.
In summary, the etiology of periodontal disease involves a complex interplay between oral bacteria, the immune system, and other risk factors. By understanding the underlying causes of the disease, patients can take steps to prevent its development and seek appropriate treatment if necessary.
Treatment:
There are several non-surgical and surgical treatments available for periodontal disease, depending on the severity of the disease and the patient's specific needs. The goal of both non-surgical and surgical treatments for periodontal disease is to remove bacteria and diseased tissue, promote healing, and restore the health and function of the gums and bone which serve as the foundation for our teeth. The specific treatment plan will depend on the severity of the disease, the patient's overall health, and other factors that may be contributing to the condition. Controlling active periodontal disease is a crucial step prior to any surgical periodontal treatment such as dental implants, crown lengthening, gum grafting, or bone grafting - maintaining periodontal health throughout your treatment will ensure a predictable and stable long-term outcome.
Non-surgical treatments:
Scaling and root planing: This is a deep cleaning procedure that removes plaque and tartar from below the gum line and smooths the root surfaces of the teeth to remove bacterial toxins. This procedure is usually performed under local anesthesia.
Antibiotics: Oral or topical antibiotics may be used in combination with scaling and root planing to reduce bacteria and inflammation.
Surgical treatments:
Flap surgery: This procedure involves lifting the gums away from the teeth to provide access for removal of tartar and bacteria and reshape the bone if necessary.
Bone Grafting and Guided tissue regeneration: If periodontal disease has caused bone loss, bone grafting may be necessary to restore the bone and provide a stable foundation for the teeth. This surgical technique involves using a barrier membrane to encourage the growth of new bone and gums in areas where they have been lost due to periodontal disease. In some cases, a gum graft may be recommended to replace gum tissue that has been lost due to periodontal disease.
Frequently asked questions:
Q: How long does periodontal (gum) surgery take?
A: The length of time for periodontal surgery can vary depending on the location and severity of the condition being treated. However, most procedures typically take between 1-2 hours.Q: Is periodontal (gum) surgery painful?
A: Periodontal surgery is usually performed by a licensed periodontist under local anesthesia, which numbs the area being treated. However, some discomfort and sensitivity may be experienced during the recovery period.Q: How long does it take to recover? Most patients go back to work the following day without needing any prescription medications. Sutures are removed after the initial healing period of 2-3 weeks.
Q: Will I need to take time off work or school after surgery?
A: Most patients are able to return to work or school the day after their procedure. However, it is recommended to avoid strenuous activity for a few days following the surgery.Q: Can periodontal (gum) surgery be prevented?
A: Maintaining good oral hygiene, such as brushing and flossing regularly, can help prevent periodontal disease from developing. However, if the disease has already progressed, a surgical intervention may provide the most definitive results.